Brief Overview of Nepal and the Health System
Nepal is a landlocked country in South Asia, located between China and India. Nepal is divided into seven provinces and 77 districts. It has a diversified geography, with the Himalayan Mountain range in the north and the lowland Terai plains in the south. Nepal had a population of approximately 29 million, comprising 48.5% males and 51.5% females. Most of the population is in the age group (15-64) years, 14% of them are children less than 14 years, and 7.7% of them are 65 years and older. The Terai region is home to more than half (50%) of the people, with 43% living in hilly areas and 6.7% in mountainous areas. Most people (83%) reside in rural areas. The annual population growth rate is 1.4% (WHO, 2025a).
Nepal is classed as a lower-middle-income (LMC) country that continues to experience developmental and health issues due to poverty, geographic limitations, and poor infrastructure (WHO, 2025a).
Historically, Nepal’s health system relied on traditional medicine like Ayurveda until 879 AD, but after that health system underwent significant transformation over the years (Rai et al., 2001). In 2015, Nepal’s health system underwent a huge reformation, and according to the new constitution, Nepal switched from a unitary system to a federal system of government.
In the present scenario, Nepal is a federal republic with three federal levels of government and a health system mainly divided into three main levels of structure: Federal, Provincial, and local levels of government. There are 753 local governments (LLGs), which range from large municipal authorities. Delivery of health services is decentralized, with distinct tasks assigned to each level of government. Specifically, the basic health services (BHS) are predominantly organized at the local level.
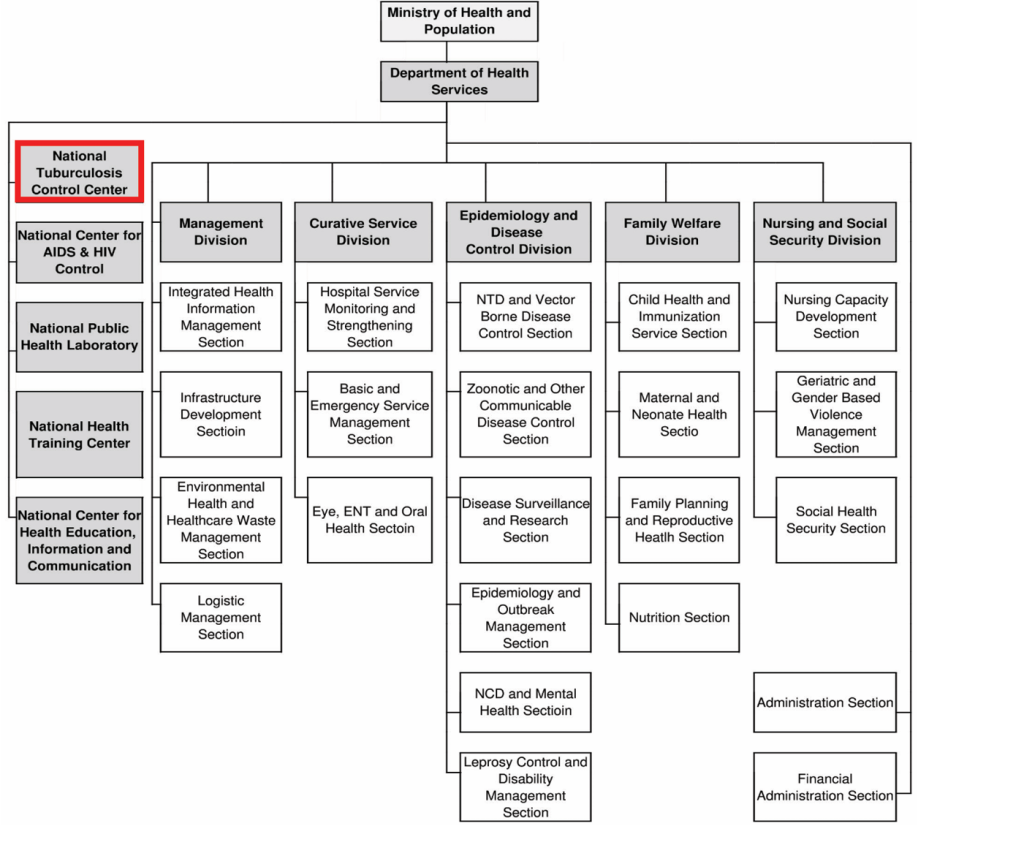
Figure 1: Structure of the Department of Health Services under MOHP
Burden of TB in Nepal
TB is one of the top ten leading causes of death in Nepal (WHO, 2025c). Though the incidence rate of TB has decreased over the years, TB is still a significant public health problem in Nepal.
In Nepal, the tuberculosis incidence (per 100,000 population) has improved by 188 cases per 100,000 from 417 [235 – 652] in 2000 to 229 [126 – 355] in 2023 (WHO, 2024).
Table 1: Nepal TB burden estimates, 2022
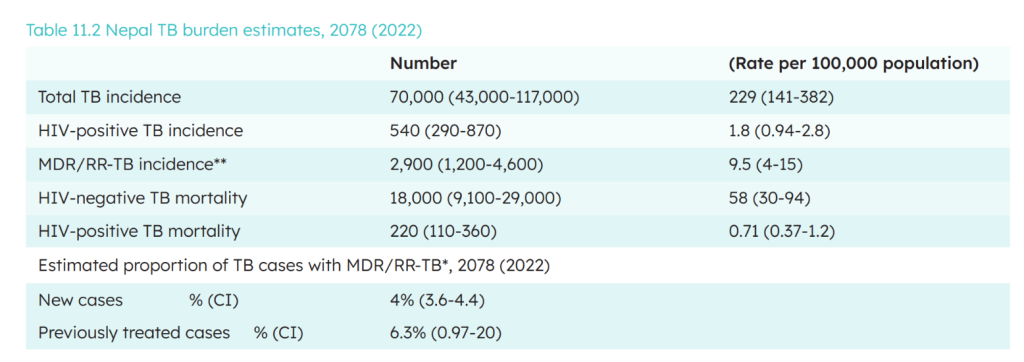
Source: Source: Nepal Tuberculosis Control Center. 2020. National Tuberculosis Prevalence Survey Report 2076 (2020). Department of Health Services, Ministry of Health and Population, Government of Nepal
Epidemiology of TB in Nepal
By geographical division, the notification rates are lowest in the mountain areas to the North of Nepal, and highest in the terai in the South. The proportion of tuberculosis cases in children (0-14 years) has slightly increased from 6.2% in 2014-15 to 7.3% in 2016-17, with variations among provinces (4%–16%) (National Tuberculosis Control Center (NTCC), 2020).
TB surveillance in Nepal
The disease under surveillance in Nepal is Tuberculosis (TB), which includes drug-sensitive TB, multidrug-resistant TB (MDR-TB), and extensively drug-resistant TB (XDR-TB). TB is an infectious disease caused by the bacterium Mycobacterium tuberculosis. TB is a significant public health issue in Nepal, being one of the leading causes mortality in Nepal.
B patients are primarily found in low- and middle-income nations like Nepal. Primarily, TB affects the lungs and spreads through the air when people are infected with TB cough, sneeze or spit (WHO, 2025b).
Tuberculosis spreads quickly in areas where people congregate or live in close quarters. People with HIV/AIDS and others with weaker immune systems are more likely to get tuberculosis than those with healthy immune systems. Risk factors for TB include people with diabetes, weakened immune system, malnutrition, tobacco use, and harmful use of alcohol (WHO, 2025b). Most common signs and symptoms of TB are prolonged cough, chest pain, weakness, fatigue, weight loss, fever, night sweats (WHO, 2025b). TB is a preventable and curable disease. To prevent TB, the vaccine called Bacillus Calmette-Guérin (BCG) is the only available vaccine that protects against the severe forms of TB, like TB meningitis.
BCG vaccination is given to children right after birth in many countries (CDC, 2025a). Inactive TB can be treated with drugs like Isonazid, Rifampicin, and Rifapentine (CDC, 2025b). Active TB can be treated with drugs like Ethambutol, Isonazid, Moxifloxacin, Rifampicin, Rifapentine, and Pyrazinamide. Depending upon the treatment plant, it takes four to nine months to treat TB with these medications (CDC, 2025b). In addition to vaccination, other preventive measures for TB include frequently washing hands, coughing into the elbow, avoiding close contact with other people, and using personal respiratory protective devices when travelling to places where TB is prevalent.
National TB Control Program
In Nepal, the National Tuberculosis Control Centre (NTCC) is the focal point of the National Tuberculosis Program (NTP) and is responsible for formulating policies, strategies, planning, monitoring, surveillance and quality assurance. NTP is a priority program oof the Government of Nepal.
Nepal’s National Tuberculosis Control Centre (NTCC) oversees TB surveillance, integrating it within the general primary healthcare system.
The TB surveillance system under NTCC has the following purposes:
- Detect and notify all TB cases promptly.
- Monitor trends in incidence, prevalence, and treatment outcomes.
- Identify high-risk populations and geographic hotspots.
- Guide public health responses, resource allocation, and policy development.
- Track progress toward national and international TB elimination targets (e.g., WHO End TB Strategy)
WHO is the key international technical agency supporting NTP to conduct TB surveillance in Nepal (Department of Health Services, 2024).
Population under surveillance
TB surveillance in Nepal focuses on all the residents of Nepal with special attention to high risk populations such as people living with HIV (PLHIV), children, symptomatic contacts of pulmonary and bacteriologically confirmed TB patients, extrapulmonary presumptive cases (from cerebrospinal fluid, lymph node, and other tissues specimen) living in slums, prisoners, internally displaced population (IDPs), migrant workers and immunocompromised patients (National Tuberculosis Control Center (NTCC), 2020).
General Design of the Surveillance System
The TB surveillance system in Nepal is designed as a case-based reporting system, using WHO-recommended tools. It includes:
- Routine case notification through public and private providers.
- Special surveys (e.g., TB Prevalence Survey).
- Electronic systems: NTPMIS (TB-specific) and HMIS (general).
Specifically, the National Tuberculosis Program Management Information System (NTPMIS) serves as an efficient online web and case-based surveillance system (Figure 2), capturing comprehensive data crucial for monitoring and evaluation.
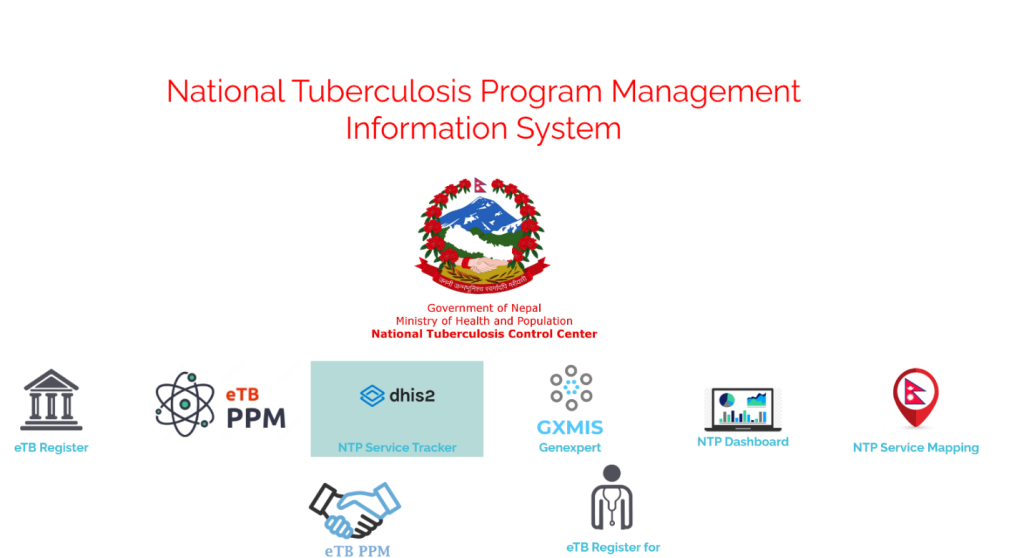
Figure 2 Web-based TB surveillance system
How the data is collected?
TB data is obtained by the NTP using the WHO standardized surveillance system. Both the Public health services and the private sectors reported TB cases to the NTP every quarter. The Health Management Information System (HMIS) is an effective tool adopted by NTP to collect data related to TB. HMIS has different reporting forms under the heading: (Tuberculosis Sample Collection Form, Tuberculosis Laboratory Register, Tuberculosis Treatment Card (Health Facility), Tuberculosis Treatment Card (Patient), Tuberculosis Treatment Register, PAL: Smoking cessation Register, DR Tuberculosis Laboratory Register, and DR Tuberculosis Treatment Register). Health workers at public institutions also report TB cases using the HMIS form.
How Data is Reported?
- All the health workers at different levels are required to report the TB routine cases, lab and patient reports via online online-based reporting system using the NTPMIS portal. HMIS reporting forms and tools are used, and data collected at local-level health facilities are compiled by the provincial TB focal point and sent to the central NTCC for analysis. NTCC also reports TB data to WHO annually through the Global TB Report submission.
- Routine TB data are reported and available on the NTPMIS portal: https://ntpmis.gov.np
- HMIS data can be accessed via the national data portal for health workers: https://hmis.gov.np/dataportal
Government health facilities (primary health care centers, hospitals), national and provincial laboratories, and private health providers are required to report TB cases, patient data, and lab reports into the established system.
SWOT Analysis of the system
Strengths
One of the strengths of the existing system is the use of nationwide electronic TB registers (NTPMIS, eTB register). It is a well-established program with the integration of the HMIS system. Although this system collects all data related to TB, however, there are still things that need to be done to improve the TB surveillance and increase case notification rates.
Challenges
Nepal’s Tuberculosis (TB) program has numerous challenges that limit its effectiveness and impact. The key challenges include the battle to acquire appropriate funds for vital TB prevention, treatment, and care (Kakchapati, 2025). The other challenges include underreporting from the private sector (Kakchapati, 2025). There exist challenges related to infrastructure issues in remote areas, like internet issues, which limit the usability of registers.
How can the system be improved?
To improve the notification gaps, the concerned authority should strengthen mandatory TB case reporting for the private sector.
More training for staff, especially in remote areas of Nepal, to get familiar with the reporting system and to fill the case notification gaps.
Talking from the public perspective, the system should be clearer, and the data should be accessible to the public about TB surveillance in Nepal. For instance, the data portal website and the National TB program’s website did not have enough information regarding how the system works. Therefore, it would be better to provide detailed information to the public.
- To improve the notification gaps, the concerned authority should strengthen mandatory TB case reporting for the private sector.
- More training for staff, especially in remote areas of Nepal, to get familiar with the reporting system and to fill the case notification gaps.
References
CDC. (2025a, January 31). Bacille Calmette-Guérin (BCG) Vaccine for Tuberculosis | Tuberculosis (TB) | CDC. https://www.cdc.gov/tb/hcp/vaccines/index.html
CDC. (2025b, April 17). Treating Tuberculosis | Tuberculosis (TB) | CDC. https://www.cdc.gov/tb/treatment/index.html
Department of Health Services. (2024). Annual Health Report. www.dohs.gov.np
Kakchapati, S. (2025, March 25). Tuberculosis in Nepal: Status, Achievement and Challenges – Herd International. https://herdint.com/tuberculosis-in-nepal-status-achievement-and-challenges/
National Tuberculosis Control Center (NTCC). (2020). NATIONAL TUBERCULOSIS PREVALENCE SURVEY REPORT 2020.
Rai, S. K., Rai, G., Hirai, K., Abe, A., & Ohno, Y. (2001). The health system in Nepal—An introduction. Environmental Health and Preventive Medicine, 6(1), 1. https://doi.org/10.1007/BF02897302
WHO. (2024, January 8). WHO Data. https://data.who.int/indicators/i/13B4226/C288D13?m49=524
WHO. (2025a). World Health Organization 2025 data.who.int, Nepal [Country overview]. https://data.who.int/countries/524
WHO. (2025b, March 1). Tuberculosis. https://www.who.int/news-room/fact-sheets/detail/tuberculosisWHO. (2025c, March 11). Active case finding for TB in high-risk areas of flood-affected municipalities. https://www.who.int/nepal/news/detail/11-03-2025-active-case-finding-for-tb-in-high-risk-areas-of-flood-affected-municipalities